A Simple and Accurate test to screen for Diabetic Peripheral Neuropathy
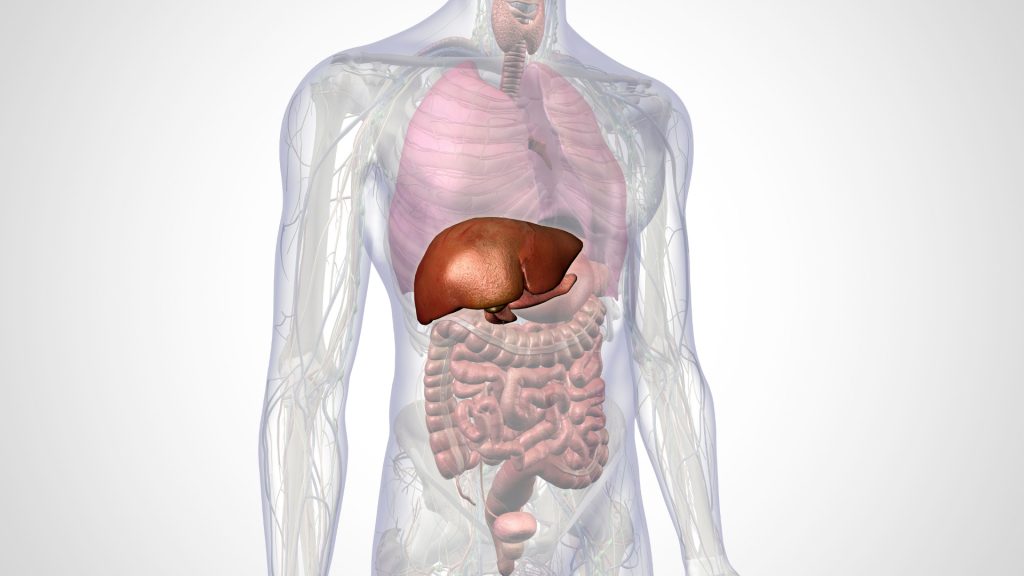
Diabetes mellitus (DM) is not only a blood sugar problem, it brings macro- and micro-vascular complications. The most common microvascular complication is diabetic neuropathy, which often damages nerves in the diabetic patient’s legs and feet. Foot assessment using Biothesiometer is a safe, quick, and reliable tool to screen and measure the progress of Diabetic peripheral neuropathy (DPN).
Diabetes mellitus (DM) is like an epidemic in the world, while it is not only a blood sugar problem, it brings macro- and micro-vascular complications. Diabetic neuropathy is the most common microvascular complication of DM, affecting as many as 50% of patients with type 1 and type 2 DM. This is actually one of the nerve disorders caused by hyperglycemia, in another word, high blood glucose. Diabetic peripheral neuropathy (DPN) involves the presence of symptoms or signs of peripheral nerve dysfunction in people with diabetes after other possible causes have been excluded. Vibration perception threshold (VPT) is considered as a gold standard for diagnosis of diabetic peripheral neuropathy which can be performed by using a biothesiometer. [1][2]
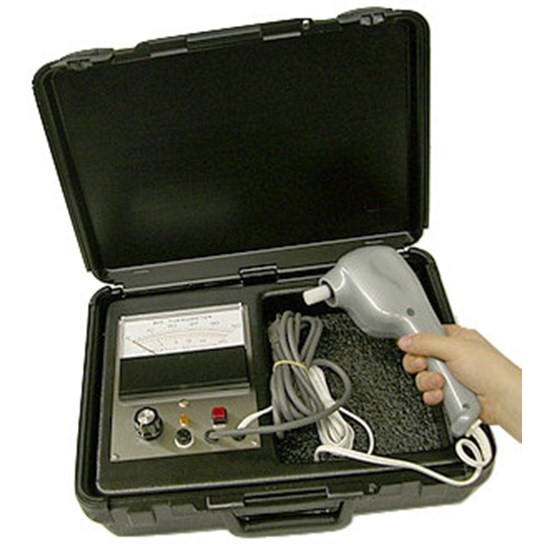
Biothesiometer is a non-invasive, quick, portable, and reliable tool to screen and measure the progress of DPN, which is commonly used in foot assessment. It responds well to assessing the vibration sensation, which is typically the first sensation that is lost in DPN. The instrument is essentially known as an “electrical tuning fork” whose amplitude may be set to any predetermined level or whose amplitude may be gradually increased until the threshold of vibratory sensation is reached. [3][4]
A 128Hz tuning fork can be applied to the tip of the hallux and bony prominence. It is important to give a non-vibrating stimulus such as touch to verify that the person is giving a positive response to the vibration sense and not just to the touch sensation. The vibratory perception threshold meter or biothesiometer is used to quantify the sensory loss and the progression of loss of nerve function by measurements at regular intervals. [4]

It is proven safe in use from children to the elderly. Simple procedure with shoes and socks/ stoking to be removed and lay supine on a couch or sat with their legs extended and resting on a chair. [5] It allows increasing the vibrating strength and measuring the threshold of vibration perception by gradually increasing the vibrations. A probe is applied on the foot, usually on the big toe. The probe can be made to vibrate at increasing intensity by tuning a dial. The person being tested indicates as soon as he/she can feel the vibration and the reading on the dial at that point is recorded. The biothesiometer has a reading from 0-50 volts. It was reported that the risk of developing a neuropathic ulcer is much higher if a person has a biothesiometer reading greater than 30-40 volts. [6]
Good blood glucose control may help prevent or delay the onset of further problems. Foot care is an important part of treatment as well. People with neuropathy need to inspect their feet daily for any injuries. Untreated injuries increase the risk of infected foot sores and amputation. Treatment also includes pain relief and other medications as needed, depending on the type of nerve damage. Smoking increases the risk of foot problems and amputation.
In summary, biothesiometer is an important device that detects peripheral neuropathy and grades its severity. Hence biothesiometer may be used to predict the future development of neuropathic foot ulcers and chances of amputations may be reduced. Prevent the preventable.
References: 1. Jayaprakash, P., Bhansali, A., Bhansali, S., Dutta, P., Anantharaman, R., Shanmugasundar, G., & Ravikiran, M. (2011). Validation of bedside methods in evaluation of diabetic peripheral neuropathy. The Indian journal of medical research, 133(6), 645–649. 2. Bloom, S., Till, S., Sönksen, P., & Smith, S. (1984). Use of a biothesiometer to measure individual vibration thresholds and their variation in 519 non-diabetic subjects. British Medical Journal (Clinical Research Ed.), 288(6433), 1793–1795. 3. International Diabetes Federation. IDF Diabetes Atlas, International Diabetes Federation. 6th Ed. Bruxelles, Belgium; 2013 4. Yang, Z., Zhang, Y., Chen, R., Huang, Y., Ji, L., Sun, F., Hong, T., & Zhan, S. (2018). Simple tests to screen for diabetic peripheral neuropathy. The Cochrane Database of Systematic Reviews, 2018(7), CD010975. https://doi.org/10.1002/14651858.CD010975.pub2 5. Davis, E. A., Jones, T. W., Walsh, P., & Byrne, G. C. (1997). The Use of Biothesiometry to Detect Neuropathy in Children and Adolescents With IDDM. Diabetes Care, 20(9), 1448–1453. doi:10.2337/diacare.20.9.1448 6. Abhilash, P., Manasa, M., Subrahmanyam, B. S., Venkateshwarlu, E., Goverdhan, P., Nagesh, A., Reddy, G. A., & Sharvana Bhava, B. S. (2016). Efficacy of Epalrestat, Duloxetine and Epalrestat in Combination with Methylcobalamine in Diabetic Peripheral Neuropathy. Romanian Journal of Diabetes Nutrition and Metabolic Diseases, 23(4), 361–367. https://doi.org/10.1515/rjdnmd-2016-0042