Each imaging modality has its pros and cons, which doctors will take into consideration when asking patients to undergo them.
A PATIENT recently approached me to know which medical imaging modality was the best to detect cancer, if any, within her. This question has always been asked and will continue to boggle the minds of many.
First and foremost, there is no universal imaging modality that can detect everything. It is also important to know what are the underlying health issues (if any), which organ is involved, what needs to be assessed and why is the imaging needed?
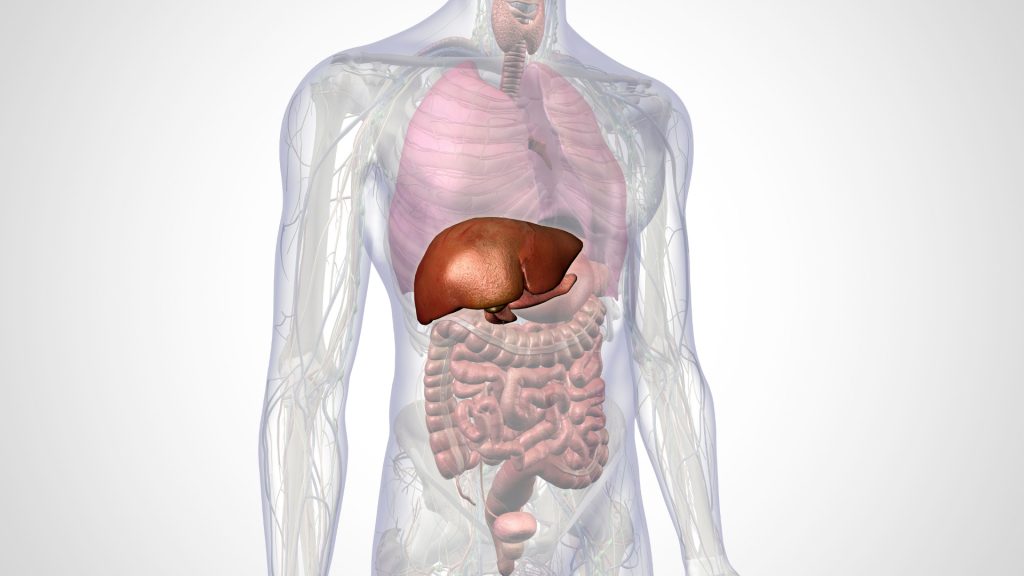
There are many medical imaging modalities available, including ultrasound, echocardiography, conventional x-rays, computed tomography (CT), magnetic resonance imaging (MRI), and nuclear medicine imaging (gamma imaging and positron emission tomography, or PET).
Each of these imaging modalities has its own strengths and weaknesses. For example, ultrasound, which basically uses attenuation and deflection of sound waves for tissue mapping, is very useful in assessing superficial soft tissue organs. Women who undergo antenatal follow-up are quite familiar with the use of this imaging modality to evaluate their baby in the womb.
However, it is difficult to get good-quality images of organs in certain areas and in obese patients with an ultrasound. The widely available conventional radiography (or more commonly known as x-ray) has been used since its first discovery by Wilhelm Roentgen in 1895. Most people will remember undergoing chest x-rays for pre-employment screening test.
On the other hand, CT scans, which also use x-rays, are able to visualize the body in 3 dimensions (3-D). This imaging modality is available in most hospitals and has become an important tool in clinical practice. It has been used to detect cerebrovascular accidents (strokes), lung diseases, cancers, and fractures. However, this scan is limited in visualizing soft tissue lesions particularly in the brain, spinal cord, and pelvic organs.
The good news is that the days where radiation from the CT machines was an issue are gone, as newer CT machines produce better quality images with much lower radiation. MRI, which uses magnetic resonance of the protons within the body, is basically free of ionizing radiation. It is able to visualize soft tissues within the body with better resolution compared to a CT scan.
Unfortunately, the lungs and bone structures are not well visualized on MRI. Patients with non-MRI compatible implants, like a non-compatible pacemaker or implantable cardioverter defibrillator (ICD), are also not allowed to undergo the scan. Fortunately, the newer generation of such implants are now MRI-compatible.
Though uncommon, the side effects related to the use of gadolinium-based contrasts – used in x-rays, CT scans, and MRIs to help visualize the targeted area – are real and the search for better alternative contrast agents is underway.
Nuclear medicine imaging
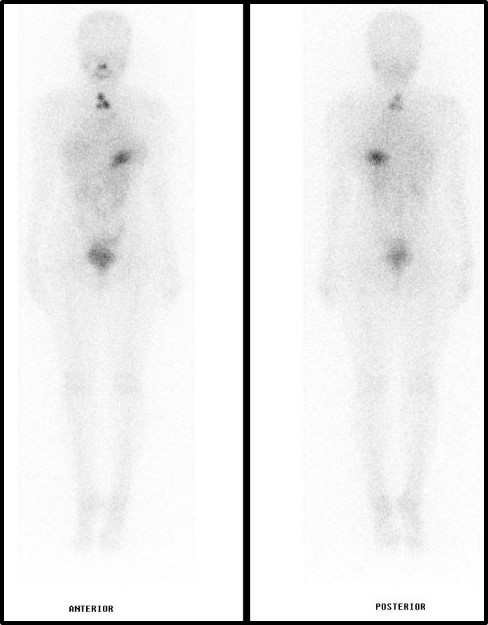
Being in the field of nuclear medicine, I am frequently asked to comment if nuclear medicine imaging is still relevant when we already have other good imaging modalities. The answer is simple: Nuclear medicine imaging has its strength in functional imaging.
In nuclear medicine imaging, small doses of radioactive substances are used either independently or paired with special pharmaceuticals to visualize the organ of interest. If doctors need to evaluate the skeletal system, a radioactive bone scan using Technetium-99m methylenediphosphonate (Tc-99m MDP) can be done.
This radiopharmaceutical will be distributed within the bones in such a way that any abnormalities will cause either an increase or decrease in its levels, which can be detected. In fact, Tc-99m MDP is so sensitive that a 5% change in bone turnover can be detected, compared to 40-50% on conventional radiographs or even a CT scan.
And early detection means early intervention.
Nuclear medicine is also unique as some radioactive substances not only treat diseases but are also able to provide images at the same time – hence the word “theranostic” – a portmanteau of “therapy” and “diagnostic”. For example, not only can radioactive iodine-131 be used for the treatment of well-differentiated thyroid cancer, but imaging of the cancer distribution can also be done – literally “killing two birds with a stone”
PET pros and cons
PET imaging is currently the “in-thing” cancer management. Whether used with CT or MRI (PET/CT or PET/MRI), the high sensitivity in the detection of cancers, and most uniquely, the determination of the level of metabolic activity within the cancer is very useful to clinicians. Though some cancers are already dead after treatment, the physical aspect of the cancer may still be seen on conventional radiographs and CT for a period of time analogous to a dead tree stump.
When dealing with cancers, time is essential and any residual metabolically active disease should be dealt with swiftly. Hence, information of the metabolic activity of the tumor is very useful – no metabolic activity means dead tissue. Furthermore, the radioactive substance can be used safely in patients with renal (kidney) impairment without causing further deterioration.
Then again, PET/CT or PET/MRI is not the ultimate imaging modality. There are limitations to using PET as not all tumors take up the radioactive substance and they might be masked by physiological uptake by normal cells.
The fear of having radioactive within the body is also a major deterrent in many patients. However, with proper counseling, they will realize that the radioactive used will basically decay exponentially and washout from the body similar to any other medical imaging contrasts.

Imaging is necessary
Once again, I highlight that no imaging modality is perfect. Not all clinical information can be gathered from non-ionizing medical imaging such as ultrasounds and MRI, and neither are all patients suitable to undergo them. Patients undergoing x-rays, CT, and nuclear medicine imaging, including PET/CT and PET/MRI, are exposed to certain levels of radiation.
Technological advancement has significantly reduced radiation exposure to the least possible, compared to many years ago. Even though the radiation exposure is minimal, many people still harbor the unfounded fear of it possibly triggering or exacerbating cancer. In actual fact, the radiation exposure from medical imaging is negligible in the course of medical treatment.
Cost is no doubt an issue in this day and age. It goes without saying that the more expensive the imaging is, the more likely patients will try to avoid it. Better equipment and technology come with a price. One needs to consider the investment, equipment costs, researches, and clinical trials involved before an imaging modality is approved for use, similar to how smartphones are being improved and made. The better the specifications of the phone, the pricier it is. But with time, prices will fall due to increasing demand and availability.
Nuclear medicine imaging is relatively expensive due to the scanner, as well as the radioactive substances needed for the imaging. These substances need to be specially ordered and are not widely available. Nonetheless, it is a small price to pay for crucial clinical information needed to manage our own health.
In short, it is important for patients to understand that doctors choose imaging modalities to help diagnose, stage, plan, evaluate and monitor their condition. There are times when doctors will order multiple imaging modalities in the course of their management. The risk and benefits for each imaging are always taken into account before subjecting patients to them. Each and every person is unique and every disease is different.
Whenever I hear patients sharing their medical conditions, I do sometimes wonder if they actually realize that they are unique individuals with different medical issues and their experience may not be applicable to their listeners. In the era of precision medicine, there is no one imaging that fits all. To achieve the best treatment, it is important to tailor the treatment according to the patient and underlying condition.
If in doubt, discuss with your doctor. I end with a quote from Ralph Waldo Emerson: “Don’t waste life in doubts and fears.”